Mental health and substance use disorders are deeply intertwined. Many people struggling with anxiety, depression, PTSD, or other conditions use substances as a coping mechanism. Alcohol, opioids, marijuana, or stimulants may provide temporary relief, but over time, they worsen mental health symptoms, increase dependency, and create a destructive cycle.
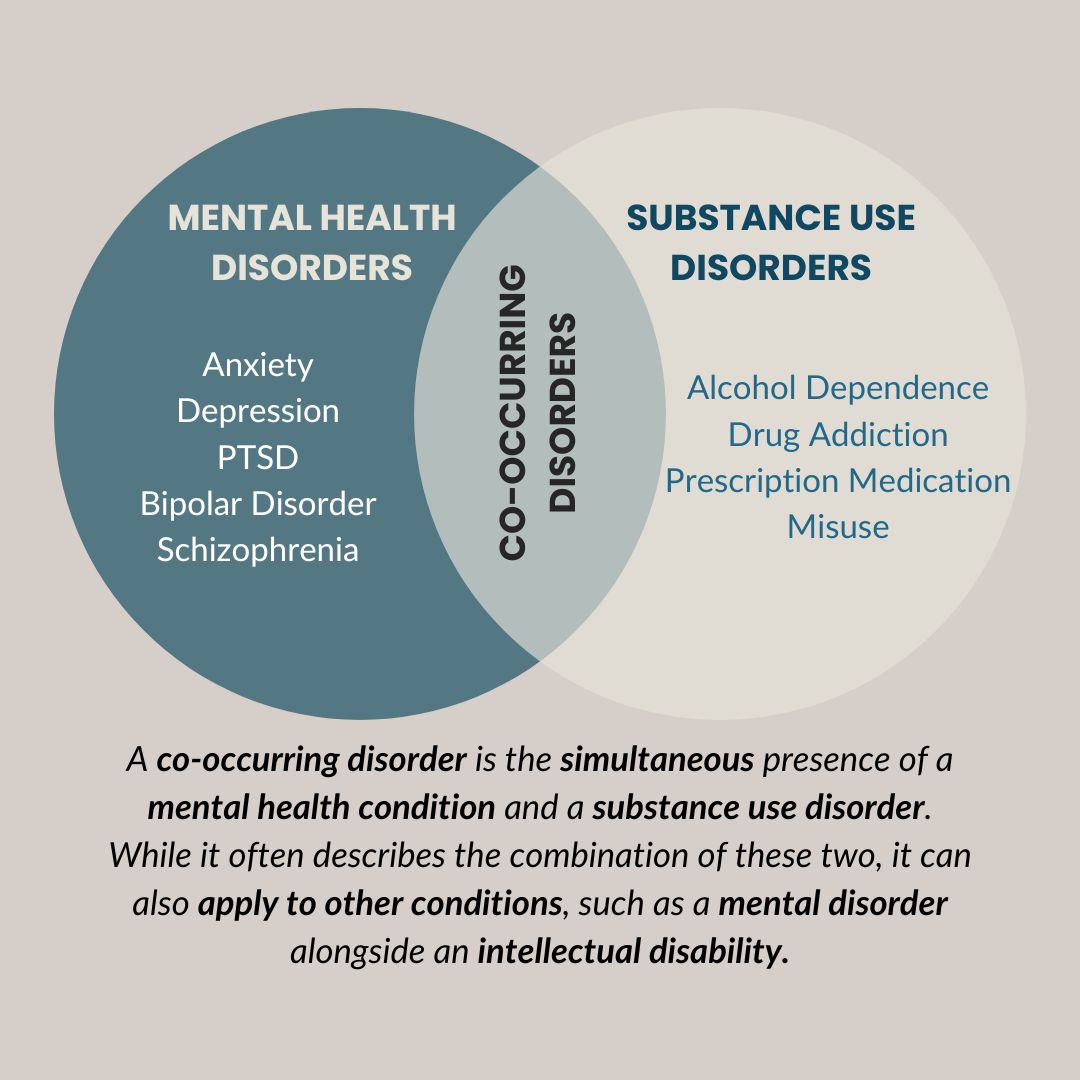
This combination of mental health disorders and substance use is known as a co-occurring disorder, or dual diagnosis. Studies show that nearly 50% of individuals with a mental health disorder will develop a substance use disorder at some point in their lives (NIDA). However, effective treatment is possible when both conditions are addressed simultaneously.
At Ridgeline Recovery, we specialize in treating co-occurring disorders by integrating addiction treatment and mental health therapy, providing individuals with a path to long-term recovery.
The Vicious Cycle: How Mental Health and Substance Use Are Connected

Mental health and substance use fuel each other, making it difficult to break free without professional help. The cycle typically looks like this:
-
A Mental Health Issue Develops → Someone experiences anxiety, depression, PTSD, or another mental health condition.
-
Substances Become a Coping Mechanism → Alcohol, prescription drugs, or illicit substances temporarily reduce stress and emotional pain.
-
Temporary Relief Leads to Long-Term Consequences → While substances numb symptoms, they also worsen brain chemistry over time.
-
Dependence and Addiction Develop → The body and mind begin relying on substances to function.
-
Both Conditions Escalate → Mental health symptoms intensify, leading to more substance use, which further deepens the addiction.
This cycle can feel impossible to escape, but with the right treatment approach, recovery is absolutely achievable. Our addiction recovery programs help individuals break this cycle by treating both addiction and mental health disorders at the same time.
Common Mental Health Disorders Linked to Substance Use
Many mental health disorders increase the risk of substance abuse. Below are some of the most common conditions that co-exist with addiction:
1. Anxiety & Substance Use
Anxiety disorders, including generalized anxiety disorder (GAD), panic disorder, and social anxiety disorder, can make daily interactions feel overwhelming. Many individuals turn to alcohol, benzodiazepines (Xanax, Valium), or marijuana to calm their nerves.
Why It’s Harmful:
-
While alcohol and drugs provide short-term relaxation, they increase anxiety over time by altering brain chemistry.
-
Benzodiazepines are highly addictive, leading to dependence, withdrawal symptoms, and worsening anxiety.
-
Marijuana can increase paranoia and panic attacks in some individuals.
2. Depression & Substance Use
Depression causes persistent sadness, fatigue, and hopelessness. Many people use alcohol, opioids, or stimulants to escape these feelings.
Why It’s Harmful:
-
Alcohol is a depressant, which means it slows brain activity and deepens depressive symptoms.
-
Opioids and stimulants (cocaine, meth) provide temporary energy boosts, but lead to severe crashes that make depression worse.
3. PTSD & Substance Use
Post-traumatic stress disorder (PTSD) affects individuals who have experienced trauma, violence, or life-threatening events. Symptoms include flashbacks, nightmares, and severe anxiety.
Why It’s Harmful:
-
Alcohol and drugs numb emotional pain, but prevent real healing.
-
Substances can intensify PTSD symptoms and lead to self-destructive behaviors.
-
Addiction therapy with trauma-informed approaches helps individuals heal without relying on substances.
4. Bipolar Disorder & Substance Use
Bipolar disorder causes extreme mood swings, from manic episodes (high energy, impulsivity) to depressive episodes (low motivation, sadness).
Why It’s Harmful:
-
Stimulants (cocaine, meth) increase impulsivity during manic episodes.
-
Alcohol and sedatives worsen depressive episodes, leading to a greater risk of self-harm or suicidal thoughts.
-
Substances interfere with mood stabilizers and make treatment less effective.
5. Schizophrenia & Substance Use
Schizophrenia affects a person’s thoughts, emotions, and perception of reality. It often involves hallucinations, paranoia, and delusions.
Why It’s Harmful:
-
Marijuana and psychedelics increase the risk of psychotic episodes.
-
Substance use interferes with schizophrenia medications, making symptoms worse.
-
Long-term addiction leads to severe cognitive decline and worsens quality of life.
The Power of Dual Diagnosis Treatment
Treating only one condition—either mental health or addiction—increases the risk of relapse. This is why dual diagnosis treatment is essential.
At Ridgeline Recovery, we use an integrated approach that includes:
1. Addiction Recovery
-
Medically supervised detox to safely remove substances from the body.
-
Inpatient and outpatient programs to prevent relapse.
-
Individualized treatment plans for long-term success.
2. Addiction Therapy
-
Cognitive Behavioral Therapy (CBT) to identify triggers and develop coping strategies.
-
Dialectical Behavior Therapy (DBT) to improve emotional regulation.
-
Trauma-informed therapy for PTSD and past trauma.
3. Addiction Treatment
-
Medication-Assisted Treatment (MAT) for opioid and alcohol addiction.
-
Family therapy to rebuild relationships damaged by addiction.
-
Support groups and aftercare programs for long-term recovery.
Coping Strategies for Long-Term Recovery
1. Develop Healthy Coping Mechanisms
-
Exercise regularly (yoga, running, weightlifting).
-
Practice mindfulness and meditation.
-
Engage in creative activities (painting, writing, music).
2. Build a Strong Support Network
-
Join support groups like Alcoholics Anonymous (AA) or Narcotics Anonymous (NA).
-
Surround yourself with positive influences who support your sobriety.
3. Prioritize Mental Health Treatment
-
Attend regular therapy sessions.
-
Take prescribed medications as directed.
-
Use stress-management techniques before cravings set in.
Breaking the Stigma: Seeking Help is Strength
Many people avoid treatment because of stigma or fear of judgment. However, mental health and addiction are medical conditions, not personal failures. Seeking help is an act of strength and self-awareness.
Key Truths About Recovery:
-
You are not alone → Millions of people struggle with co-occurring disorders and recover.
-
Treatment works → Evidence-based programs provide real solutions.
-
Your past does not define you → A healthier future is possible with the right help.
Take the First Step – Contact Us Today
Struggling with mental health and addiction can feel overwhelming, but help is available. At Ridgeline Recovery, we create personalized treatment plans to help individuals break free from addiction and regain control of their lives.
If you or someone you love needs support, contact us today. Recovery starts now.